Abstract
Background:
Diffuse large B-cell lymphoma (DLBCL) is the most common subtype of non-Hodgkin lymphoma. Although R-CHOP is nowadays considered the standard of care for DLBCL, there are still approximately 40% of patients with refractory disease or relapse, especially in the first two years. For these patients aggressive strategies as stem-cell transplantation is an option. Yet, this approach is not feasible for all patients.
Our study's aim was to examine the efficacy and safety of maintenance therapy compared to observation in patients with DLBCL after achieving complete (CR) or partial response (PR) following induction therapy.
Methods:
Systematic review and meta-analysis of randomized controlled trials including patients with DLBCL who achieved CR or PR after first line treatment with chemotherapy +/- rituximab and comparing maintenance therapy with observation or placebo. The Cochrane Library, MEDLINE, conference proceedings and references were searched until June 2017. Two reviewers appraised the quality of trials and extracted data. Primary outcome was overall survival (OS). Secondary outcomes included all-cause mortality at 1 year, relapse rate, disease control (which include progression-free survival, event-free survival, and disease-free survival) and safety.
For each trial, results were expressed as relative risks (RR) with 95% confidence intervals (CI) for dichotomous data and hazard ratios (HRs) and variances for time-to-event outcomes. We assessed heterogeneity using the I2 measure of inconsistency. Statistically significant heterogeneity was defined as p-value < 0.1 or I2 > 50%. We conducted the meta-analysis using a fixed-effect model, which assumes a similar effect measure between studies and is appropriate when no significant clinical and statistical heterogeneity is present. Random-effects model was used in analyses with significant heterogeneity (I2 > 50%).
Results:
Our search yielded 14 trials conducted between the years 1981 and 2016, including 3677 patients. In six and in two trials rituximab was added to all and to half of the patients receiving induction therapy, respectively. Median age of patients in the trials was 49 to 70 years. Nine trials included patients at any international prognostic index (IPI) while four of them included patients with intermediate-high and high risk age-adjusted IPI.
Regarding maintenance therapy: seven trials included rituximab as the maintenance therapy, three included Interferon alfa as maintenance, two included immunomodulatory drugs (thalidomide and lenalidomide), one trial included cyclophosphamide and prednisone, and one included the serine threonine kinase inhibitor enzastaurin.
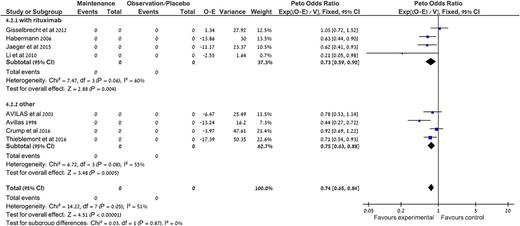
Data from nine trials was available for analysis of OS. Maintenance treatment did not improve OS compared to observation, HR 0.98, [95% confidence interval (CI) 0.85-1.13, I2=0, 2980 patients]. Results were the same in a subgroup analysis by the type of maintenance (rituximab vs. other). Maintenance therapy did not decrease all-cause mortality at 1 year, RR 1.01 [95% CI 0.82-1.24, I2=0]. However, it decreased relapse rate, HR 0.78, [95% CI 0.65-0.93, I2=52, random effects model] and improved disease control compared to observation, HR 0.74, [95% CI 0.65-0.84, I2=51, random effects model]. Disease control was significantly improved in the subgroup of studies evaluating rituximab as maintenance, HR 0.73, [95% CI 0.59-0.90, I2=60, random effects model].
Regarding safety, five trials reported serious or grade III/IV adverse events. These adverse events were significantly more common in the maintenance compared to observation, RR=1.72, [95% CI 1.26-2.33. I2=75%]. In addition, neutropenia and infections grade III/IV were significantly higher in the maintenance arm, RR=2.03 [95% CI 1.49-2.76, I2=44%] and RR=1.89 [95% CI 1.08-3.29, I2=0%] respectively.
Conclusions:
Maintenance therapy in patients with DLBCL achieving CR or PR after induction therapy did not change OS, yet it decreased relapse rate and improved disease control at the cost of a higher infection rate.
Out data does not support routine administration of maintenance therapy in patients with DLBCL. Further research is needed to define subgroups which may benefit the most from this therapy.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal